Keywords
Abstract
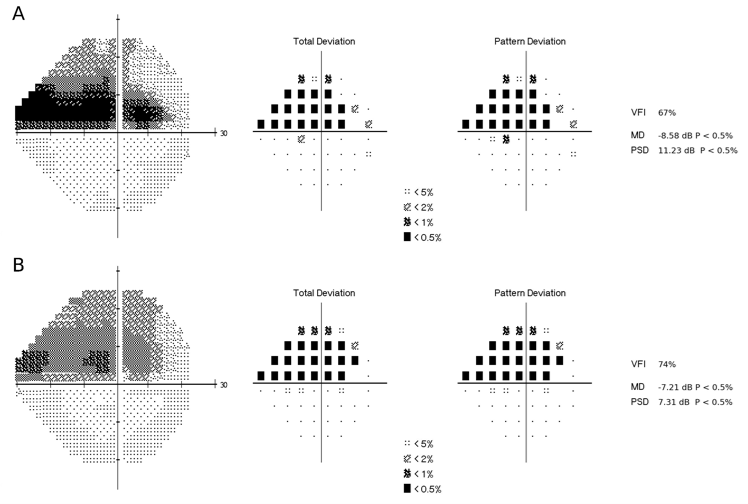
The relationship between structural damage and functional loss in glaucoma is of great importance for its diagnosis and management. The functional status is usually assessed through visual field examination, a subjective test that is burdensome and time-consuming. Moreover, it depends on patients’ answers and there is a learning curve until accurate and reliable measurements are possible. Structural assessment, on the other hand, has remarkably improved since the development of optical coherence tomography, a fast test that allows for objective and quantitative analysis of retinal layers. The relationship between the two tests, however, is complex and nonlinear, and is influenced by interindividual variability. Thus, qualitative evaluation or the use of conventional statistics might not be appropriate. In recent years, we have seen a remarkable evolution of artificial intelligence algorithms and deep learning models. These techniques have proved adequate to model such complicated relationships. In this review, we summarize studies that investigate the structure and function relationship in glaucoma making use of artificial intelligence and deep learning, the challenges associated with predicting visual field information from structural measurements, and the strategies adopted to improve their accuracy.
References
Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA. 2014;311(18):1901-1911. https://doi.org/10.1001/jama.2014.3192
Artes PH, Iwase A, Ohno Y, Kitazawa Y, Chauhan BC. Properties of perimetric threshold estimates from Full Threshold, SITA Standard, and SITA Fast strategies. Invest Ophthalmol Vis Sci. 2002;43(8):2654-2659.
Gardiner SK, Swanson WH, Goren D, Mansberger SL, Demirel S. Assessment of the Reliability of Standard Automated Perimetry in Regions of Glaucomatous Damage. Ophthalmology. 2014;121(7):1359-1369. https://doi.org/https://doi.org/10.1016/j.ophtha.2014.01.020
Kuang TM, Zhang C, Zangwill LM, Weinreb RN, Medeiros FA. Estimating Lead Time Gained by Optical Coherence Tomography in Detecting Glaucoma before Development of Visual Field Defects. Ophthalmology. 2015;122(10):2002-2009. https://doi.org/10.1016/j.ophtha.2015.06.015
Christopher M, Bowd C, Belghith A, et al. Deep Learning Approaches Predict Glaucomatous Visual Field Damage from OCT Optic Nerve Head En Face Images and Retinal Nerve Fiber Layer Thickness Maps. Ophthalmology. 2020;127(3):346-356. https://doi.org/10.1016/j.ophtha.2019.09.036
Garway-Heath DF, Poinoosawmy D, Fitzke FW, Hitchings RA. Mapping the visual field to the optic disc in normal tension glaucoma eyes. Ophthalmology. 2000;107(10):1809-1815.
Yu H-H, Maetschke SR, Antony BJ, et al. Estimating Global Visual Field Indices in Glaucoma by Combining Macula and Optic Disc OCT Scans Using 3-Dimensional Convolutional Neural Networks. Ophthalmology Glaucoma. 2021;4(1):102-112. https://doi.org/https://doi.org/10.1016/j.ogla.2020.07.002
George Y, Antony BJ, Ishikawa H, Wollstein G, Schuman JS, Garnavi R. Attention-Guided 3D-CNN Framework for Glaucoma Detection and Structural-Functional Association Using Volumetric Images. IEEE Journal of Biomedical and Health Informatics. 2020;24(12):3421-3430. https://doi.org/10.1109/JBHI.2020.3001019
Huang X, Sun J, Majoor J, et al. Estimating the Severity of Visual Field Damage From Retinal Nerve Fiber Layer Thickness Measurements With Artificial Intelligence. Transl Vis Sci Technol. 2021;10(9):16. https://doi.org/10.1167/tvst.10.9.16
Zhu H, Crabb DP, Garway-Heath DF, editors. A Bayesian Radial Basis Function Model to Link Retinal Structure and Visual Function in Glaucoma. 3rd International Conference on Bioinformatics and Biomedical Engineering 2009 11-13 June 2009; Beijing, China.
Zhu H, Crabb DP, Schlottmann PG, et al. Predicting Visual Function from the Measurements of Retinal Nerve Fiber Layer Structure. Investigative Ophthalmology & Visual Science. 2010;51(11):5657-5666. https://doi.org/10.1167/iovs.10-5239
Guo Z, Kwon YH, Lee K, et al. Optical Coherence Tomography Analysis Based Prediction of Humphrey 24-2 Visual Field Thresholds in Patients With Glaucoma. Invest Ophthalmol Vis Sci. 2017;58(10):3975-3985. https://doi.org/10.1167/iovs.17-21832
Mariottoni EB, Datta S, Dov D, et al. Artificial Intelligence Mapping of Structure to Function in Glaucoma. Transl Vis Sci Technol. 2020;9(2):19. https://doi.org/10.1167/tvst.9.2.19
Datta S, Mariottoni EB, Dov D, Jammal AA, Carin L, Medeiros FA. RetiNerveNet: using recursive deep learning to estimate pointwise 24-2 visual field data based on retinal structure. Scientific Reports. 2021;11(1):12562. https://doi.org/10.1038/s41598-021-91493-9
Park K, Kim J, Lee J. A deep learning approach to predict visual field using optical coherence tomography. PLoS One. 2020;15(7):e0234902. https://doi.org/10.1371/journal.pone.0234902
Park K, Kim J, Kim S, Shin J. Prediction of visual field from swept-source optical coherence tomography using deep learning algorithms. Graefes Arch Clin Exp Ophthalmol. 2020;258(11):2489-2499. https://doi.org/10.1007/s00417-020-04909-z
Shin J, Kim S, Kim J, Park K. Visual Field Inference From Optical Coherence Tomography Using Deep Learning Algorithms: A Comparison Between Devices. Transl Vis Sci Technol. 2021;10(7):4. https://doi.org/10.1167/tvst.10.7.4
Raza AS, Cho J, de Moraes CG, et al. Retinal ganglion cell layer thickness and local visual field sensitivity in glaucoma. Arch Ophthalmol. 2011;129(12):1529-1536. https://doi.org/10.1001/archophthalmol.2011.352
Lee JW, Morales E, Sharifipour F, et al. The relationship between central visual field sensitivity and macular ganglion cell/inner plexiform layer thickness in glaucoma. Br J Ophthalmol. 2017;101(8):1052-1058. https://doi.org/10.1136/bjophthalmol-2016-309208
Sugiura H, Kiwaki T, Yousefi S, Murata H, Asaoka R, Yamanishi K. Estimating Glaucomatous Visual Sensitivity from Retinal Thickness with Pattern-Based Regularization and Visualization. Proceedings of the 24th ACM SIGKDD International Conference on Knowledge Discovery & Data Mining; London, United Kingdom: Association for Computing Machinery; 2018. p. 783–792.
Hashimoto Y, Asaoka R, Kiwaki T, et al. Deep learning model to predict visual field in central 10° from optical coherence tomography measurement in glaucoma. Br J Ophthalmol. 2021;105(4):507-513. https://doi.org/10.1136/bjophthalmol-2019-315600
Xu L, Asaoka R, Kiwaki T, et al. Predicting the Glaucomatous Central 10-Degree Visual Field From Optical Coherence Tomography Using Deep Learning and Tensor Regression. Am J Ophthalmol. 2020;218:304-313. https://doi.org/10.1016/j.ajo.2020.04.037
Asano S, Asaoka R, Murata H, et al. Predicting the central 10 degrees visual field in glaucoma by applying a deep learning algorithm to optical coherence tomography images. Sci Rep. 2021;11(1):2214. https://doi.org/10.1038/s41598-020-79494-6
Hashimoto Y, Kiwaki T, Sugiura H, et al. Predicting 10-2 Visual Field From Optical Coherence Tomography in Glaucoma Using Deep Learning Corrected With 24-2/30-2 Visual Field. Translational Vision Science & Technology. 2021;10(13):28-28. https://doi.org/10.1167/tvst.10.13.28