Keywords
Abstract
Purpose: To examine the relationship between the cardiovascular status and variations in optical coherence tomography (OCT)-derived parameters of the peripapillary and macular tissues, and macular vascular flow area measured by optical coherence tomography angiography (OCTA) in healthy subjects.
Design: Prospective, open-label, non-randomized clinical study.
Methods: Twenty one eyes of 21 healthy subjects were analyzed using a swept-source device, including OCT and OCTA acquisitions. Cardiovascular changes were investigated by performing a practical hand-grip test (HGT). Blood pressure, heart rate, OCT and OCTA structural and vascular changes were measured and analyzed before and after the HGT-induced exercise.
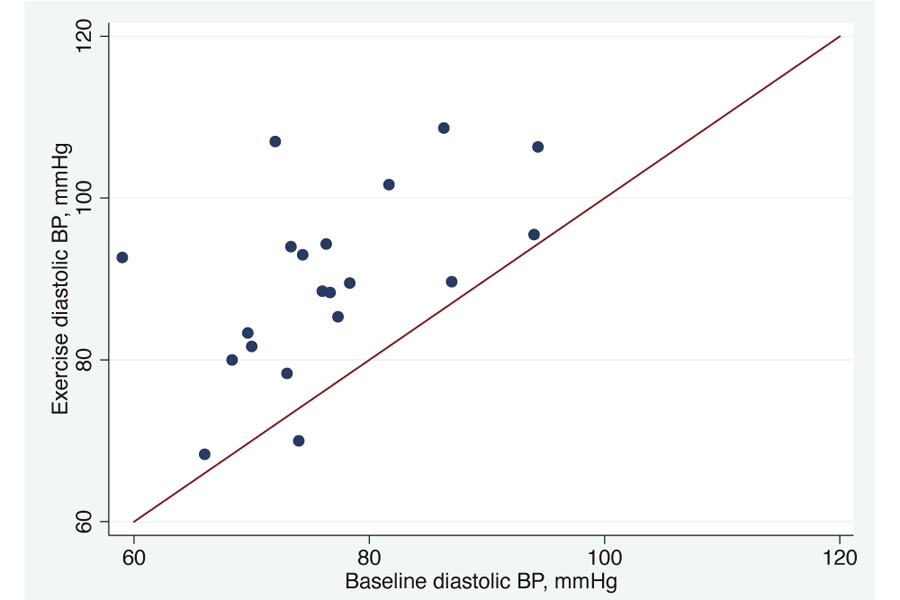
Results: The mean patient age was 34.0 (± 15.2) years. While both diastolic and systolic blood pressures increased significantly aft er exercise (p < 0.001 and p = 0.003, respectively), the heart rate did not show a significant increment (p = 0.182). OCT structural parameters of the optic nerve did not change significantly. Instead, a significant redistribution of choroidal thickness (CT) was observed in the macular region, with a significant reduction (-6.5%, p = 0.001) in the outer-nasal macular sector after exercise. OCTA acquisitions did not show changes in the vascular density of both the superficial retinal layer and deep retinal layer.
Conclusions: We demonstrated that HGT-induced exercise can moderately elevate blood pressure without detectable effects on OCTA-derived parameters in healthy young subjects. Moreover, it produced a significant redistribution of CT. Further studies are needed to better explain the possible role of HGT in the characterization of the pathophysiology of ocular diseases associated with abnormalities of the vascular function such as glaucoma, age-related macular degeneration, and diabetic retinopathy.
References
Funk RH. Blood supply of the retina. Ophthalmic Res. 1997;29(5):320–325.
Causin P, Guidoboni G, Malgaroli F, Sacco R, Harris A. Blood flow mechanics and oxygen transport and delivery in the retinal microcirculation: multiscale mathematical modeling and numerical simulation. Biomech Model Mechanobiol. 2016;15(3):525–542.
Wei X, Balne PK, Meissner KE, Barathi VA, Schmetterer L, Agrawal R. Assessment of flow dynamics in retinal and choroidal microcirculation. Surv Ophthalmol. 2018;63(5):646–664.
Verticchio Vercellin AC, Cutolo CA, Dellafiore C, Lava M, Tinelli C, De Silvestri A, et al. Inter-device reproducibility of retrobulbar blood flow velocity measurements in healthy subjects using color Doppler imaging. J Ultrasound. 2016;1–6.
Kouadio AA, Jordana F, Koffi NJ, Le Bars P, Soueidan A. The use of laser Doppler flowmetry to evaluate oral soft tissue blood flow in humans: A review. Arch Oral Biol. 2018;86:58–71.
Popa-Cherecheanu A, Schmidl D, Werkmeister RM, Chua J, Garhöfer G, Schmetterer L. Regulation of Choroidal Blood Flow During Isometric Exercise at Different Levels of Intraocular Pressure. Invest Ophthalmol Vis Sci. 2019;60(1):176–182.
Schmidl D, Schmetterer L, Witkowska KJ, et al. Factors Associated With Choroidal Blood Flow Regulation in Healthy Young Subjects. Invest Ophthalmol Vis Sci. 2016;57(13):5705–5713.
Calzetti G, Fondi K, Bata AM, et al. Assessment of choroidal blood flow using laser speckle flowgraphy. Br J Ophthalmol. 2018;102(12):1679–1683.
Leitgeb RA, Werkmeister RM, Blatter C, Schmetterer L. Doppler Optical Coherence Tomography. Prog Retin Eye Res. 2014;41:26–43.
Kashani AH, Chen C-L, Gahm JK, Zheng F, et al. Optical coherence tomography angiography: A comprehensive review of current methods and clinical applications. Prog Retin Eye Res. 2017;60:66–100.
Koustenis A, Harris A, Gross J, Januleviciene I, Shah A, Siesky B. Optical coherence tomography angiography: an overview of the technology and an assessment of applications for clinical research. Br J Ophthalmol. 2017;101(1):16–20.
Rodríguez FJ, Staurenghi G, Gale R, Vision Academy Steering Committee. The role of OCT-A in retinal disease management. Graefes Arch Clin Exp Ophthalmol. 2018;256(11):2019–2026.
Alnawaiseh M, Lahme L, Treder M, Rosentreter A, Eter N. Short-term effects of exercise on optic nerve and macular perfusion measured by optical coherence tomography angiography. Retina. 2017;37(9):1642.
Cardillo Piccolino F, Lupidi M, Cagini C, et al. Retinal Vascular Reactivity in Central Serous Chorioretinopathy. Invest Ophthalmol Vis Sci. 2018;59(11):4425–4433.
Kallioinen N, Hill A, Horswill MS, Ward HE, Watson MO. Sources of inaccuracy in the measurement of adult patients’ resting blood pressure in clinical settings: a systematic review. J Hypertens. 2017;35(3):421–441.
Komma S, Chhablani J, Ali MH, Garudadri CS, Senthil S. Comparison of peripapillary and subfoveal choroidal thickness in normal versus primary open-angle glaucoma (POAG) subjects using spectral domain optical coherence tomography (SD-OCT) and swept source optical coherence tomography (SS-OCT). BMJ Open Ophthalmol. 2019;4(1):e000258.
Akahori T, Iwase T, Yamamoto K, Ra E, Terasaki H. Changes in Choroidal Blood Flow and Morphology in Response to Increase in Intraocular Pressure. Invest Ophthalmol Vis Sci. 2017;58(12):5076–5085.
Harris A, Arend O, Bohnke K, Kroepfl E, Danis R, Martin B. Retinal blood flow during dynamic exercise. Graefes Arch Clin Exp Ophthalmol. 1996;234(7):440–444.
Iester M, Torre PG, Bricola G, Bagnis A, Calabria G. Retinal Blood Flow Autoregulation after Dynamic Exercise in Healthy Young Subjects. Ophthalmologica. 2007;221(3):180–185.
Bill A, Sperber GO. Control of retinal and choroidal blood flow. Eye. 1990;4(2):319–325.
Kur J, Newman EA, Chan-Ling T. Cellular and physiological mechanisms underlying blood flow regulation in the retina and choroid in health and disease. Prog Retin Eye Res. 2012;31(5):377–406.
Martin CE, Shaver JA, Leon DF, Thompson ME, Reddy PS, Leonard JJ. Autonomic Mechanisms in Hemodynamic Responses to Isometric Exercise. J Clin Invest. 1974;54(1):104–115.
Bata AM, Fondi K, Witkowska KJ, et al. Optic nerve head blood flow regulation during changes in arterial blood pressure in patients with primary open-angle glaucoma. Acta Ophthalmol (Copenh). 2019;97(1):e36–41.
Kim SV, Semoun O, Pedinielli A, Jung C, Miere A, Souied EH. Optical Coherence Tomography Angiography Quantitative Assessment of Exercise-Induced Variations in Retinal Vascular Plexa of Healthy Subjects. Invest Ophthalmol Vis Sci. 2019;60(5):1412–1419.
Bond V, Curry BH, Adams RG, Obisesan T, Pemminati S, Gorantla VR, et al. Cardiovascular Responses to an Isometric Handgrip Exercise in Females with Prehypertension. North Am J Med Sci. 2016;8(6):243–249.
Walamies M, Turjanmaa V. Assessment of the reproducibility of strength and endurance handgrip parameters using a digital analyser. Eur J Appl Physiol. 1993;67(1):83–86.
Khurana RK, Setty A. The value of the isometric hand-grip test-studies in various autonomic disorders. Clin Auton Res. 1996;6(4):211–218.
Vera J, Jiménez R, Redondo B, Torrejón A, De Moraes CG, García-Ramos A. Effect of the level of effort during resistance training on intraocular pressure. Eur J Sport Sci. 2019;19(3):394–401.